By Dr. Brook Alemayehu (Internist)
After the observation by Lei Fang and colleagues that coronaviruses use ACE2 to target cells (especially type II alveolar cells), the same protein is likely to be involved for SARS-COV-2.
The findings that more than 80% of total ACE2 expression was found in AT2 cells are thought to explain the severe alveolar injury phenomenon observed after COVID-19 infection . An early study showed that ACE2 shows 42% homology with ACE, but the substrate specificity and enzymatic activity of the two enzymes are quite different.
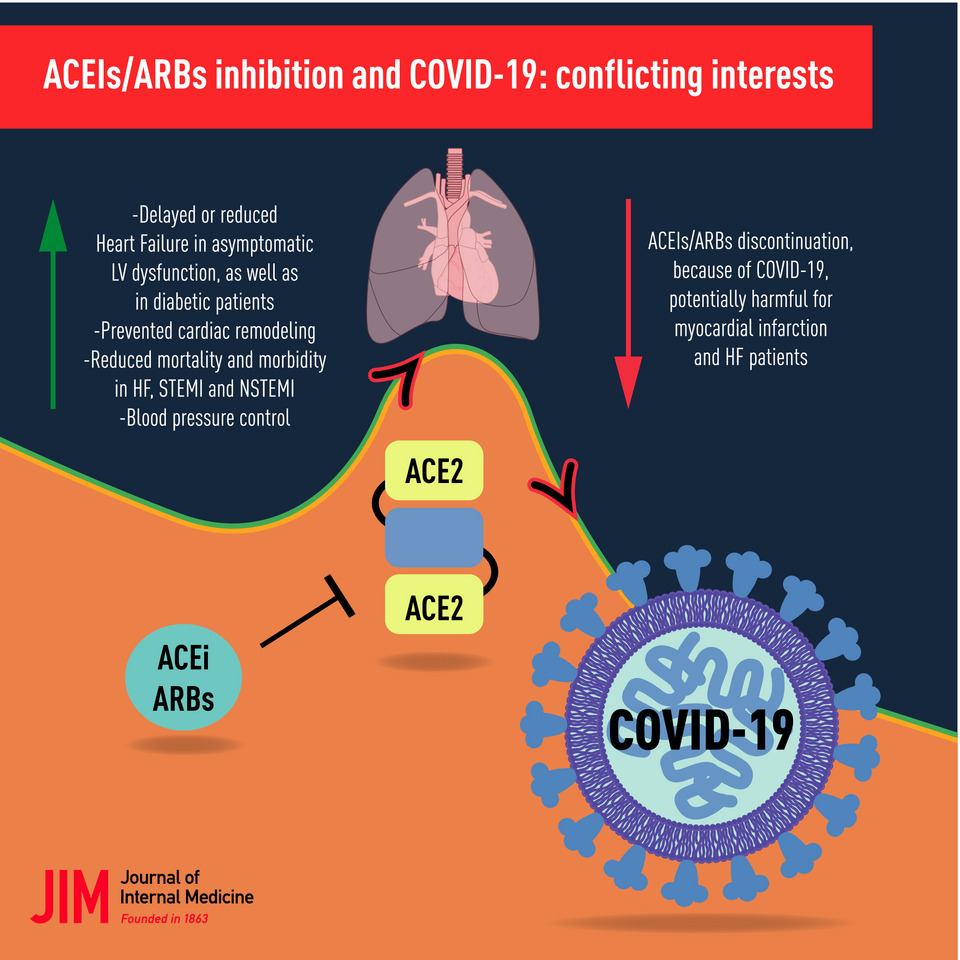
With the assumption that ACE2 is up-regulated by Angiotensin-converting enzyme inhibitors (ACEIs) and Angiotensin receptor blockers (ARBs), it was suggested that alternative treatment should be sought for those at high risk of infection.
This has led to increasing uncertainty and concern among the public and professionals about the use of RAAS inhibitors in such patients
It should be highlighted, though, that the data in humans are too limited to support or refute these hypotheses and concerns and that the following points should be given adequate attention.
1. Over-representation of Hypertension
In the largest case series from China, hypertension was the most frequent coexisting condition with an estimated prevalence of 15%; which is actually lower than the prevalence in the general population in China.
However, coexisting conditions, including hypertension, have consistently been reported to be more common among patients with COVID-19 who have had severe illness, been admitted to the ICU, received mechanical ventilation, or died than among patients who have had mild illness.
2. Hypertension tracking with Age
Most comorbidities, especially hypertension, appear to track closely with advancing age which is emerging as the strongest predictor of COVID-19–related death
Unfortunately, reports to date have not rigorously accounted for age or other key factors that contribute to health as potential confounders in risk prediction.
3. Uncertain Effects of RAAS Inhibitors on ACE2 in Humans
Despite substantial structural homology between ACE and ACE2, their enzyme active sites are distinct. As a result, ACE inhibitors in clinical use do not directly affect ACE2 activity
Experimental animal models have shown mixed findings with respect to the effects of ACE inhibitors on ACE2 levels or activity in tissue.
4. Potential for Benefit Rather Than Harm of RAAS Blockers in COVID-19
In a small study, patients with COVID-19 appeared to have elevated levels of plasma angiotensin II, which were in turn correlated with total viral load and degree of lung injury.
Restoration of ACE2 through the administration of recombinant ACE2 appeared to reverse this devastating lung-injury process in preclinical models of other viral infections (H5N1 & RSV) and safely reduced angiotensin II levels in a phase 2 trial evaluating acute respiratory distress syndrome in humans.
5. Correlation between ACE2 expression and Severity of viral infection?
- A recent study revealed that SARS-CoV was not isolated from patients with high expression of ACE2, which suggested that the viral infection process may require other receptors or cofactors.
- In addition, further studies are needed to clarify whether hypertensive drugs alter the gene expression and activity of ACE2 in human lung tissues, thus affecting the disease outcome of novel coronavirus pneumonia.
6. Risk of Discontinuation of RAAS Inhibition
RAAS inhibitors have established benefits in protecting the kidney and myocardium, and their withdrawal may risk clinical decompensation in high-risk patients.
And this apparent potential for harm related to withdrawal of these agents should be taken into consideration as well.
Conclusion
On the basis of the available evidence, many speciality societies have come to recommend that RAAS inhibitors should be continued in patients in otherwise stable condition who are at risk for, are being evaluated for, or have COVID-19.
The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease.
In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation.
The ESC (European Society of Cardiology) Council on Hypertension strongly recommended that physicians and patients should continue treatment with their usual anti-hypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACEi or ARBs should be discontinued because of the COVID-19 infection.